“Chylomicrons are the dominant lipoprotein in blood after eating a fatty meal. Chylomicrons deliver dietary lipids to extra-intestinal tissues. Because chylomicrons are secreted into the lymphatic system rather than the blood, they are difficult to isolate and purify, especially in humans. As a result, their role as a symptom and driver of metabolic disease is potentially under-appreciated. Our goal is to understand the role of chylomicrons in disease, and to determine dietary and pharmacologic approaches to ameliorating this dysfunction. ”
Key questions in our lab:
1. How do Foxp3+Tregs choose between lipoprotein triglyceride and plasma free fatty acids for fuel and does this metabolic flexibility change Treg function, proliferation, or maintenance of Foxp3?
2. What is the role of dysfunctional chylomicrons in Cystic Fibrosis metabolic disease, and how does modulator therapy (Trikafta®) impact chylomicron metabolism?
3. What are the mechanisms of lymph versus portal partitioning during the absorption the nutrients, and is this regulated in health and disease?
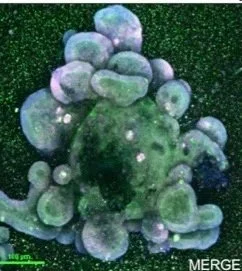
Small intestinal organoids as a model of dietary lipid absorption.
Chylomicrons are difficult to isolate, and the intestine is notoriously finicky to study. We use primary intestinal organoids to get around these issues.
Mesenteric Lymph Collection:
We have pioneered a unique 1-day mouse lymph cannulation model that enables the collection of flowing mesenteric lymph from live mice for 6-h after a duodenal nutrient infusion. This makes us one of the only lab’s in the world to collect post-prandial lymph in >50ul quantities. We have now extended this mouse surgical model to include a quadruple cannulation, with cannulas in the duodenum, jugular vein, portal vein, and mesenteric lymph duct.